 BBC
BBCA woman who used her life savings to have vaginal mesh removed in the United States said she could no longer wait for surgery in Northern Ireland after passing blood and debris.
Sylvia Vickery, 61, said she was “angry and sad” but had no other choice as waiting lists to be seen and treated at the Belfast Mesh Clinic were too long.
One operating day a month is allocated for the removal of mesh in Belfast, however, with only two surgeries on average taking place each day, some women have been waiting years.
The Belfast Trust said there had been 38 pelvic mesh surgery removals in the past five years.
 Sylvia Vickery
Sylvia VickeryAbout 53 women are currently on an outpatient waiting list, while 47 are waiting for surgery.
Ms Vickery, who is from Eglinton in County Londonderry, likened her pain to “shards of glass rubbing against her organs” which was “excruciating” especially when passing urine, or even when walking.
She spent more than £20,000 to have the mesh removed which included the private surgery and travel costs to St Louis, Missouri, in the US.
Ms Vickery had vaginal mesh implants at Altnagelvin Hospital in 2014 to treat urinary stress incontinence.
In March 2023, she began to feel a burning sensation in her lower stomach and felt extreme pain, especially when passing urine.
She recalled one episode when she spent 45 minutes in her bathroom.
“There was just so much blood in the toilet bowl and I noticed I had passed a piece of the mesh which felt like it was cutting through me.
“The pain was excruciating, I felt I was going to pass out,” Ms Vickery said.
What is vaginal mesh?
Surgical mesh which is used to support the vagina and organs including the bladder, the rectum, or the urethra.
Vaginal mesh implants are described as medical devices – hernia mesh is used in men.
Mesh was considered to be the gold standard treatment for incontinence and prolapse in women for years.
However, the net-like implant can erode and harden, cutting through tissue causing serious pain and damage to organs.
Some women were left in permanent pain, unable to walk, work or have sex.
As concerns grew about the scale of complications the routine use of mesh was paused and then suspended in 2018.
Ms Vickery attended a private clinic in Northern Ireland where a scan revealed the mesh had perforated her bladder.
Her GP made an urgent referral to Altnagelvin, where a secretary told her it could be up to eight months before she would be seen at the Belfast Mesh Clinic.
It was set up in 2018 to treat women from across Northern Ireland.
Unable to cope with the pain, Ms Vickery decided to travel to see a specialist in St Louis in April 2024.
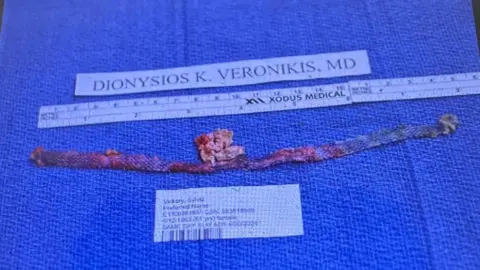
During her surgery, a piece of mesh measuring nearly 20cm long was removed.
“I had to be opened from hip to hip to allow the surgeon to view all the mesh and begin the repairs,” she said.
“The surgeon said I was a very lucky lady and if I had waited any longer to be treated the damage could have been even more serious.
“The mesh had gone into my bladder. It was a massive repair job – the surgery took two and half hours longer than expected.”
 Sylvia Vickery
Sylvia VickeryIt is unclear exactly how many women in Northern Ireland are adversely impacted by mesh implants.
While for many the operation has been successful, it’s thought that hundreds require removal.
According to an NI Audit report, between 1998 and 2018, there were about 11,000 total vaginal mesh implants carried out in Northern Ireland with a conservative estimate of between 5-10% experiencing problems.
The audit found data was not properly collated within the local health trusts.
Sling the Mesh NI has 603 members – a majority said they were experiencing problems.
Four months on from her surgery Ms Vickery said she felt 10 years younger.
“I have no issues at this moment, my recovery was fantastic I was able to fly and return home 10 days after the operation,” she said.
Sylvia said she is fortunate to have a supportive husband and family.
According to the local mesh groups, Mesh Ireland and Sling the Mesh, mesh can destroy lives and relationships.
“When it comes to mesh and surgical removal women are being let down,” Ms Vickery said.
“The length of time women are having to wait to be seen and then treated is just too long, there is very little happening in Belfast’s mesh clinic.”
In England, between April 2021 and October 2022, 393 patients have received surgery, while the average waiting time for a first outpatient appointment was 15 weeks, and 23 weeks for surgery.
Note:- (Not all news on the site expresses the point of view of the site, but we transmit this news automatically and translate it through programmatic technology on the site and not from a human editor. The content is auto-generated from a syndicated feed.))




